Last Modified: 06/14/2023
Diagnostic Audiology Appendix

Appendix A
Risk indicators associated with permanent congenital, delayed-onset, or progressive hearing loss in childhood
(Risk indicators that are marked with an asterisk are of greater concern for delayed-onset hearing loss.)
- Caregiver concern* regarding hearing, speech, language, or developmental delay.
- Family history* of permanent childhood hearing loss
- Neonatal intensive care of >5 days, or any of the following regardless of length of stay: ECMO,* assisted ventilation, exposure to ototoxic medications (gentamycin and tobramycin) or loop diuretics (furosemide/lasix), and hyperbilirubinemia (jaundice) requiring exchange transfusion.
- In-utero infections, such as CMV,*, herpes, rubella,syphilis,and toxoplasmosis.
- Craniofacial anomalies, including those involving the pinna, ear canal, ear tags, ear pits, and temporal bone anomalies.
- Physical findings, such as white forelock, associated with a syndrome known to include a sensorineural or permanent conductive hearing loss.
- Syndromes associated with hearing loss or progressive or late-onset hearing loss,* such as neurofibromatosis,osteopetrosis, and Usher syndrome). Other frequently identified syndromes include Waardenburg, Alport, Pendred, and Jervell and Lange-Nielson.
- Neurodegenerative disorders,* such as Hunter syndrome, or sensory motor neuropathies, such as Friedreich ataxia and Charcot-Marie-Tooth syndrome.
- Culture-positive postnatal infections associated with sensorineural hearing loss,* including confirmed bacterial and viral (especially herpes viruses and varicella) meningitis.
- Head trauma, especially basal skull/temporal bone fracture* requiring hospitalization.
- Chemotherapy*
Figures A, B, & C show an infant during an ABR procedure.

A.

B.

C.
The audiologist measures the infant’s auditory response by placing electrodes (sensor disks) on the infant’s scalp to determine if there is electrical energy generated by the auditory nerve in response to the signal. The signal is delivered through insert earphones or ear muffins (air conduction) and then a vibrator on the skull (bone conduction). The audiologist measures the baby’s air conduction and bone conduction thresholds (the lowest, softest-intensity levels at which a repeatable response is obtained) and then evaluates the nerve’s response to sounds presented at a variety of intensity levels for each ear. In order for the audiologist to determine how well an infant hears different frequencies (configuration of the hearing loss) he/she must use a combination of tone bursts (frequency-specific stimuli) in the threshold measurements.
Appendix B
What can parents do to improve the outcome of the diagnostic auditory brainstem response test (ABR) for their infant?
Unsedated
- Keep your infant awake until quite late the night before the hearing test (sleep deprived) so that he/she will sleep soundly during the evaluation. A quiet, sleeping baby allows the examiner to get better responses to the ABR testing.
- Try to feed your infant just prior to the testing to ensure a relaxed, comfortable, and sleepy baby. (In most cases, this can be done at the facility the ABR will be administered and just prior to the test.)
- Bring a blanket or stuffed toy that your infant is familiar with to make him/her more comfortable during the evaluation.
- Allow for a block of time in your schedule for the audiologist to test the infant.(Sometimes more time is needed for the evaluation if the infant does not want to quiet down and sleep right away.)
Sedated
- Complete the informed consent given to you for the sedation to take place.
- Keep your infant awake until quite late the night before the hearing test (sleep deprived) so that he/she will sleep soundly during the evaluation. A sleep-deprived infant with the sedation medication provided will better ensure a quiet, sleeping baby.
- Bring a blanket or stuffed toy that your infant is familiar with to make him more comfortable during the evaluation.
- Follow your audiologist’s instructions very carefully on what the baby may eat prior to the evaluation. Usually restrictions for eating are spelled out in the instructions given to you for the procedure. If you do not get this information or do not understand the instructions, be sure to ask what the policies are for your infant.
- Do Not Give Your Infant Any Sedation Prior to Arriving for the Abr! A professional should administer this so that your infant’s vital signs can be monitored carefully.
- Allow for a block of time in your schedule for the audiologist to test the infant.(Sometimes more time is needed for the evaluation if the infant does not want to quiet down and sleep right away.)
Figure D shows an infant during an OAE procedure

D.
There are two basic types of clinical measures of OAEs: transient evoked Otoacoustic emissions (TOAE) and distortion product Otoacoustic emissions (DPOAE). Both are easily measured in infants and children making them an important component of the audiological test battery.
Figure E shows an infant during tympanometry

E. (Baby picture by
Mid-ear lab)
Although professionals other than the pediatric audiologist (such as the Ear Nose and Throat doctor (ENT) or the Primary Care Physician (PCP) may perform tympanometry it is not likely that they have equipment with a high frequency probe tone and so reliable results will not be obtained for infants between 0 and 6 months of age. It is important that a high frequency probe tone is routinely used to increase the reliability and accuracy of tympanometry measures in the age group (0-6 months of age).
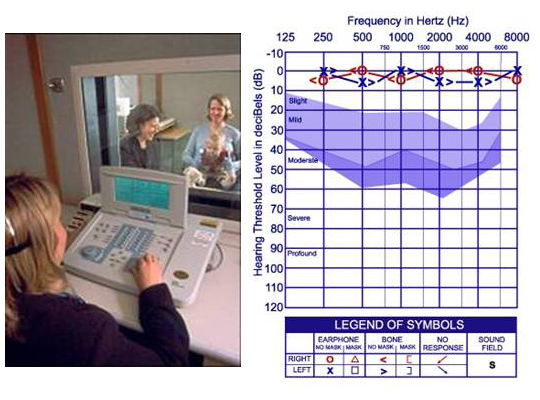
Figure F shows an infant during behavioral Audiological testing and a typical audiogram
Hearing loss can be displayed on the audiogram comparing air and bone conduction responses at different frequencies. Air conduction thresholds are measured with (insert) earphones. Therefore, if there is a problem anywhere in the auditory system (outer, middle, or inner ear), these thresholds will be poorer than normal.
F.
Figure G shows an infant during bone conduction testing (Picture courtesy Boys Town National Research Hospital)

G.
Bone conduction thresholds are measured by placing a small vibrator on the mastoid bone (the bony part behind the external ear). When sound is presented via bone conduction, it bypasses the outer and middle ear and goes directly to the inner ear. Therefore, the only problem that is detected by bone conduction is a problem in the inner ear.